ALREADY CLEANING OR STILL POLISHING?
Caries and periodontitis are avoidable. Dental plaque resulting from microbial colonisation of tooth surfaces is seen as an aetiological factor for caries and periodontitis, the most common infectious diseases in the Western world. Biofilms are complex 3-D structures in which, for example, bacteria are encased in a mucoid extracellular matrix. They do not just occur in the oral cavity, but on all boundary surfaces that are moist and warm. Their significance regarding the occurrence of problems such as periodontitis and caries has been scientifically acknowledged. Science has been trying for years to find efficient means and methods to remove and prevent biofilm. Although we have new findings on biofilm, we are still using instruments and materials from a time when the aetiology revolved around sub- and supragingival calculus. Why do we first remove calculus with hand instruments and electric scalers despite the focus falling here on living biofilm? Why do we still polish with rubber cups and brushes, which are proven to harm hard- and soft-tissue? Why do we use four methods to remove biofilm: ultrasound, rubber cups, hand instruments and polishing compound? Is there not just one method that is completely painless, more effective and saves time?
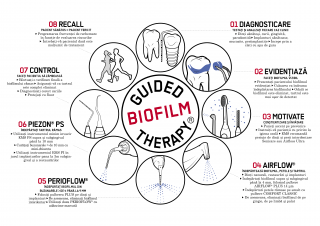
What is GBT? It is very simple: GBT is my concept for success, a procedural protocol, divided into several steps that are easy to explain. They are establishment of findings, disclosing; patient education, including performance of oral hygiene at home; remotivation of the patient; sub- and supragingival biofilm management with the appropriate instruments, gentle treatment that is really necessary; quality control; recommendations; and individual assessment of the recall interval.
In GBT, it is especially important to disclose the tooth deposits that cause harm. It is what the clinician discovers here that guide the clinician when performing oral prophylaxis. This is how we achieve optimum results for the benefit of patients, treating them with the least invasive method while ensuring maximum comfort. GBT is suitable for healthy patients, including children; patients with orthodontic appliances; and those with caries, gingivitis, periodontitis, peri-implant mucositis or peri-implantitis.
What GBT means for me
GBT has changed not just my work procedures, but also me personally. I have been a dental hygienist for 18 years and also work as a dental coach at the Swiss Dental Academy. In my seminars, I place importance on individual prophylactic treatment concepts. I do not concentrate solely on removing calculus, but also on biofilm. After all, it should be the task of the team at the dental surgery to offer optimum, personalised prophylactic treatment for lifelong oral health. At the surgery, we should apply an individual concept that combines the latest findings with a better quality of life for the patient and greater earnings for the dentist. For me, this concept is GBT. Since I learnt about GBT, my work tray has undergone a radical change. I need fewer instruments, but use the ones I have far more effectively. I too have changed. From being a cheerful sort of person anyway, I have now become even happier. I enjoy my work more and see how patients are willing to come back. After all, they have just received gentle treatment, as well as had an informative discussion about personal oral hygiene with me. I see how happy patients feel, and how happy I feel as well.
THE EIGHT STEPS OF GBT
What is the secret of GBT? In a nutshell: hand instruments and traditional polishing make way for ultrasonic instrumentation PIEZON NO PAIN and AIRFLOW with low-abrasion erythritol-based PLUS powder. GBT combines these technologies in eight successive treatment steps.
Step 1: Findings
We perform no treatment without thorough screening for caries and periodontal disease, which we accomplish using conventional tests, for example periodontal screening index, approximal plaque index and sulcus bleeding index. To ensure exact reproducibility of the indices, it is advisable for the entire prophylaxis team at the dental surgery to agree on documenting and evaluating their findings according to one specific index and system.
We need to know whether the patient takes medication, suffers from systemic disease (e.g. diabetes), has a pacemaker or possibly has any allergies. The anamnesis must be clarified in detail. The data filtered here allows us to decide which technical instruments and materials can be used during the prophylaxis session without putting the health of the patient or the clinician at risk. Visual inspection of the patient’s teeth is followed by examination of the mucosa in the oral cavity. It is important to note that, before treatment, we always start by administering a mouthwash to protect both the patient and the clinician.
Step 2: Disclosing
Coloured biofilm is the best way to show patients the correct cleaning action (techniques) in their individual case. We use disclosing agent to motivate them. By making biofilm visible to patients, they understand their problems better, and this is proven to result in greater compliance. Disclosing helps the clinician even more. We are able to target biofilm more accurately and increase the success of its removal. Studies have shown that, without disclosing, some 20 per cent of biofilm is left in place, particularly when it is supragingival. Only clinicians who use disclosing agent are able to remove up to 100 per cent of supragingival deposits. This also means that, if there is nothing there, it does not have to be removed. In the past, we cleaned every tooth, but left half the deposits behind.
Step 3: Motivation and oral hygiene instruction
Motivation is the driving force behind patient satisfaction. Disclosing is thus the basis for successful instruction and motivation of patients to perform oral hygiene at home. Only when patients understand their situation will they remain motivated. Motivation and personalised instruction are therefore a central and exacting element of GBT. For oral hygiene at home, I recommend using suitable aids that are individually tailored to the patient’s needs.
I strongly recommend Philips Sonicare toothbrushes (31,000 brush head movements), and Philips AirFloss owing to its dynamic sonic technology and minimally invasive efficacy. The success of patients in cleaning their teeth using these technologies or a combination of them after instruction leads to excellent results in terms of oral hygiene. I have seen even greater success as regards stabilisation, particularly in the case of patients with periodontal disease or unsatisfactory lifestyles.
Step 4: AIRFLOW
We first remove the biofilm. Why the biofilm first? It is very simple: as already mentioned above, calculus has never caused disease on its own. The main reason for many problems in the oral cavity is the quality of the biofilm, and its adverse processes and effects—far-reaching, even affecting the entire body. If we remove the biofilm first, we are eliminating bacteria and so stopping disease.
We can also remove stains successfully with an efficient procedure that has been learnt. Deposits of all kinds, including calculus, are identified more easily while working, becoming visible both supra- and subgingivally. This allows us to target them more accurately in our work. We protect our patients from being treated unnecessarily. That should be a consideration of all treatments performed on patients.
We consider more carefully what instruments are in fact necessary and select them accordingly. We should step in only where there is a real need for treatment. It is now easy to remove young calculus and stains. We are gentler on the patient in our work. It has now become possible to apply an approach that is extremely gentle, minimally invasive, atraumatic and precisely targeted to the specific problems of each patient. This new cleaning technology is also effective when teeth are malaligned or very close together, and with surfaces that are not easily accessible and impossible to reach with a polishing cup and brush. We can also clean the tongue and palate. If the necks of the teeth are exposed, we can likewise deal with this without damaging the cementum or dentine.
Whether a patient has gingivitis, periodontitis or periimplantitis: AIRFLOW and PLUS powder allow us to work subgingivally down to a sulcus depth of up to 4 mm. Anyone who has ever caught rubber cups on orthodontic appliances and then administered a powder–water treatment jet will not want to do without this new method.
Step 5: PERIOFLOW
When it comes to removing subgingival biofilm, in 4 to 9 mm periodontal and peri-implant pockets, I recommend using PERIOFLOW. The PERIOFLOW nozzle has enabled the treatment of millions of periodontal pockets, and we have achieved excellent results in the case of peri-implantitis, for example. I recommend using it six to eight weeks after initial therapy. When doing so, it is important to ensure you do not work horizontally on the tooth and the pocket, but pocket by pocket, proceeding slowly and without pressure, ensuring an extremely gentle action. Working vertically is necessary here.
Step 6: PIEZON
If calculus is present, I opt for the latest technology: PIEZON. PIEZON NO PAIN is based on piezoceramic energy conversion of linear movements. Hand instruments are overshadowed here. PIEZON is not only highly precise, but also intelligent and minimally invasive. The PS tip is ideal for supra- and subgingival application, while the PI instrument can also be used on titanium or ceramic surfaces. The instrument is moved over the surface of the teeth without applying pressure (the PS instrument is held parallel to the tooth surface), to avoid any loss of tooth substance or changes to surface structures. Patients find this procedure very pleasant.
Step 7: Control
We must check that we have removed all biofilm and calculus. This is what patients expect of a professional in our field. I recommend performing this check with a fine probe and a pair of dental loupes. The chemical plaque check is followed by final examination and final diagnosis by the dentist.
Step 8: Recall
Our aim is long-term stabilisation, preservation of tooth substance and avoidance of disease. This will only succeed with regular recall. The patient should leave the dental surgery with a recall appointment, which must be scheduled at once based on the findings. This depends on numerous individual factors and risks, which include the patient’s general anamnesis, diet, reconstructions,
anatomical structures, cleaning habits and general state
of oral hygiene.
Conclusion
We should ask ourselves every day: What is the efficacy and benefit of each method? What is the effect of cleaning? What are the clinical parameters like? How much time can I take? What safety does the method offer me with hard- and soft-tissue and restoratives? What level of comfort can I offer patients? How do I guarantee the health of my patients? Hand instruments and conventional polishing do not provide satisfactory solutions, but GBT is already able to do so.
GBT is a scientific concept for success at every dental surgery, offering intelligent guidance for every clinician. GBT is not only a safe and reliable procedure that smooths your path toward success, it also ensures even better treatment and dental prophylaxis results. I recommend that your entire team at the surgery try out GBT once—you will be delighted with it.